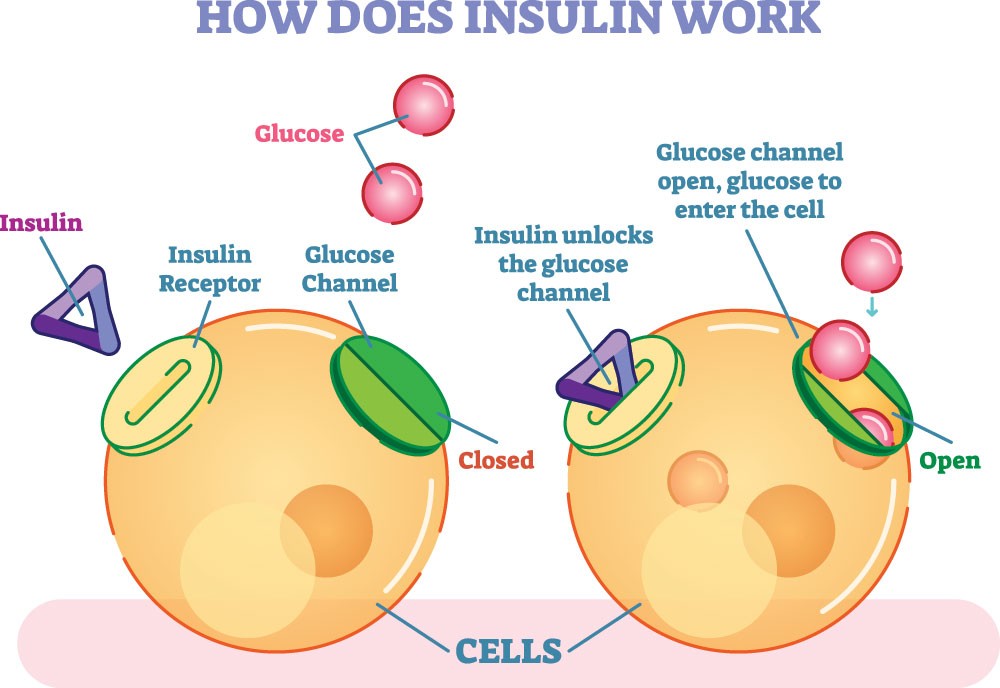
Insulin is a hormone produced by the pancreas that allows glucose to enter cells in muscles, fat, and the liver, where it’s used for energy. Insulin resistance occurs when cells become less responsive to insulin, resulting in higher blood sugar levels. In response, the pancreas produces more insulin to help glucose enter cells, creating an excess insulin condition.
When the pancreas can no longer keep up with this demand, blood sugar levels remain high, leading to prediabetes and, eventually, type 2 diabetes.

Why Does Insulin Resistance Lead to Higher Insulin Production?
In individuals with insulin resistance, the body’s cells stop responding effectively to insulin. To combat this, the pancreas ramps up insulin production to maintain normal blood sugar levels. This overproduction of insulin may temporarily keep blood sugar levels under control, but it often comes at the cost of exhausting pancreatic beta cells, which leads to reduced insulin production capacity over time.
If left unaddressed, this cycle can increase the risk of developing full-blown diabetes.

Symptoms and Causes of Insulin Resistance
Insulin resistance often develops gradually and can go unnoticed for years. Understanding its symptoms and underlying causes is essential for early detection and effective management.
Symptoms of Insulin Resistance
Insulin resistance can silently progress over years without showing clear signs, often leading individuals to be unaware of the condition. However, there are several symptoms that may hint at its presence:
Increased Hunger and Thirst:
According to the Cleveland Clinic, people with insulin resistance may experience intense hunger, known as polyphagia, and frequent thirst (polydipsia). High insulin levels, produced as the pancreas attempts to overcome the body’s resistance to insulin, can cause rapid fluctuations in blood sugar. These fluctuations often lead to intense cravings and a persistent feeling of hunger, even after eating. Frequent thirst may accompany this, as the kidneys work to filter excess sugar from the bloodstream.
Fatigue:
One of the hallmark signs of insulin resistance is chronic fatigue. Because insulin resistance impairs the body’s ability to use glucose for energy effectively, cells don’t receive the energy they need. As a result, people with insulin resistance often feel tired or sluggish, even after a full night’s sleep or after eating.
Weight Gain, Especially Around the Abdomen:
Insulin resistance is closely linked with obesity, particularly abdominal or visceral fat. According to the National Institutes of Health, the risk of developing diabetes and insulin resistance increases as body fat (measured by BMI) rises, from lean individuals to those who are obese. This suggests that the amount of body fat directly affects insulin sensitivity, with higher fat levels being linked to lower sensitivity across a wide range of people.
This type of fat, which accumulates around the midsection, has been associated with higher insulin levels and inflammation. High insulin levels encourage fat storage, especially around the belly, making it more challenging for people with insulin resistance to lose weight.
Frequent Urination:
Known as polyuria, frequent urination is often a response to high blood sugar levels. When glucose levels are high, the kidneys work overtime to filter and excrete the excess sugar through urine. This process leads to increased urination and may cause dehydration if not managed, creating a cycle of thirst and frequent urination.
Darkened Skin Patches (Acanthosis Nigricans):
As per the NIH, acanthosis nigricans is a skin condition commonly associated with insulin resistance. It causes dark, thick, and often velvety patches of skin that typically appear on body folds, such as the neck, underarms, elbows, knees, and knuckles. These patches result from excess insulin circulating in the body, which stimulates skin cells to reproduce more rapidly. Although harmless, acanthosis nigricans can be an early warning sign of insulin resistance, particularly in individuals with a family history of diabetes or obesity.
Each of these symptoms provides a clue to the presence of insulin resistance, but because they can also be associated with other health conditions, insulin resistance often goes undiagnosed until more severe issues arise. If you recognize several of these symptoms, consulting a healthcare provider for an evaluation may help in early detection and intervention.
Read More: Sliding Scale Insulin Therapy Chart For Diabetics
Causes of Insulin Resistance

Insulin resistance doesn’t usually result from one single cause but rather a combination of factors, including lifestyle, genetics, and underlying health conditions. Here are some key contributors:
Genetics:
Family history plays a significant role in the likelihood of developing insulin resistance. If close relatives, such as parents or siblings, have diabetes, the genetic predisposition increases. This genetic influence may affect how the body responds to insulin, making certain individuals more susceptible to insulin resistance from an early age.
Obesity:
Oxford Academic says that excess body fat, particularly in the abdominal area, is a major risk factor for insulin resistance. Fat cells, especially those around the abdomen, release chemicals that can interfere with insulin’s effectiveness. This type of fat, known as visceral fat, is metabolically active and can promote chronic inflammation, making insulin regulation more challenging.
Lack of Physical Activity:
A sedentary lifestyle can significantly reduce the body’s ability to use glucose effectively. Regular physical activity improves insulin sensitivity by helping muscles use glucose more efficiently. When activity levels are low, the muscles do not demand as much glucose, which can lead to higher blood sugar levels and ultimately strain insulin function.
High-Carbohydrate Diets:
Diets high in refined sugars and processed carbohydrates can lead to frequent spikes in blood sugar, causing the pancreas to produce more insulin. Cleveland Clinic says that highly processed foods require more insulin. Over time, the body may become less responsive to insulin as it struggles to manage consistently high sugar levels. Diets rich in whole grains, lean proteins, and healthy fats, on the other hand, support more stable blood sugar levels.
Chronic Inflammation:
Inflammation in the body, often a result of obesity, poor diet, or chronic stress, is another contributor to insulin resistance. Inflammatory markers can disrupt the signaling pathways of insulin, making it harder for cells to respond. This low-grade, ongoing inflammation creates a feedback loop where insulin resistance and inflammation worsen each other over time.
Complications of Untreated Insulin Resistance
If left untreated, insulin resistance can lead to a host of complications:
Type 2 Diabetes:
The most common complication, as insulin resistance reduces the pancreas’s ability to produce adequate insulin.
Heart Disease:
Insulin resistance is associated with high blood pressure and cholesterol, increasing the risk of heart disease.
Fatty Liver Disease:
High insulin levels contribute to fat accumulation in the liver, leading to non-alcoholic fatty liver disease.
PCOS:
Women with insulin resistance are at higher risk for polycystic ovary syndrome (PCOS), a hormonal disorder that can affect fertility.
Kidney Damage:
High blood sugar levels can damage blood vessels in the kidneys over time.
The Progression from Insulin Resistance to Diabetes
Insulin resistance often progresses from prediabetes to type 2 diabetes over time. Here’s how this transition typically happens:
Prediabetes:
Elevated blood sugar levels, but not high enough for a diabetes diagnosis.
Beta Cell Dysfunction:
As the pancreas becomes exhausted from overproducing insulin, beta cells start to fail.
Diabetes Diagnosis:
When the pancreas can no longer produce sufficient insulin to maintain normal blood glucose levels, type 2 diabetes develops.
Do Diabetics Have High Insulin Levels?
The relationship between diabetes and insulin levels can vary depending on the type and stage of diabetes.
In type 2 diabetes, many people have high insulin levels in the early stages due to insulin resistance. As the disease progresses, insulin levels may drop as the pancreas becomes less efficient at producing it.
In type 1 diabetes, insulin levels are low from the beginning due to an autoimmune attack on the insulin-producing beta cells. People with type 1 diabetes depend on external insulin to regulate blood sugar levels.
Insulin Levels in Type 1 vs. Type 2 Diabetes
Insulin plays a crucial role in managing blood sugar levels, but its behavior differs significantly between type 1 and type 2 diabetes. Type 1 diabetes involves an autoimmune attack on insulin-producing cells, leading to minimal insulin production. In contrast, type 2 diabetes begins with high insulin levels due to resistance but can progress to a deficiency over time.
Type 1 Diabetes:
- Insulin Production: Severely limited or absent due to autoimmune destruction of the pancreatic beta cells.
- Dependence on Insulin Therapy: Individuals require external insulin through injections or pumps to regulate blood glucose.
- Onset and Progression: Typically diagnosed in childhood or young adulthood, insulin production remains low throughout life.
Type 2 Diabetes:
- Initial Insulin Levels: Often elevated initially, as the pancreas tries to compensate for insulin resistance in body tissues.
- Progression Over Time: Insulin production may decrease as the pancreas becomes overworked, leading to possible insulin therapy.
- Management Evolution: Early stages may be managed with lifestyle changes and medications to improve insulin sensitivity; however, insulin injections may be needed if beta cell function declines.
Read More: Top Sugar Free Tablets List for Diabetes Patients
Lifestyle Choices to Improve Insulin Sensitivity
Adopting healthy lifestyle changes can significantly improve insulin sensitivity and reduce the risk of progression to diabetes.
- Consuming low-glycemic foods like whole grains, vegetables, and lean proteins helps regulate blood sugar levels and reduce insulin spikes.
- Increasing fiber intake with foods like fruits, vegetables, and legumes can improve blood sugar control and keep you feeling fuller for longer.
- Limiting processed foods and added sugars prevents rapid rises in blood sugar and promotes steadier insulin levels.
- Engaging in regular physical activity, such as walking, cycling, or swimming, encourages muscles to use glucose more effectively, reducing insulin resistance.
- Strength training exercises help build muscle, which increases the body’s capacity to absorb glucose and improves insulin sensitivity.
- Losing excess weight, particularly around the abdomen, can significantly reduce insulin resistance and improve overall metabolic health.
Medical Treatments to Regulate Insulin in Diabetics
For individuals managing diabetes, various medical treatments are available to help regulate insulin levels and enhance blood sugar control. These treatments vary based on the type of diabetes and the individual’s needs.
Metformin:
One of the most commonly prescribed medications for Type 2 diabetes, metformin works by reducing the liver’s glucose production and enhancing the body’s sensitivity to insulin. It helps the cells respond better to insulin, making it easier for glucose to enter cells and lower blood sugar levels.
SGLT2 Inhibitors:
These medications, such as canagliflozin and dapagliflozin, lower blood sugar by blocking the reabsorption of glucose in the kidneys. As a result, excess glucose is excreted through urine. SGLT2 inhibitors have the added benefit of helping with weight loss and reducing blood pressure, making them beneficial for individuals with Type 2 diabetes who also struggle with these issues.
GLP-1 Agonists:
GLP-1 receptor agonists, like liraglutide and semaglutide, mimic a natural hormone that encourages the pancreas to release insulin in response to high blood sugar. They also slow down gastric emptying, which helps reduce post-meal blood sugar spikes and supports better long-term glucose control. GLP-1 agonists can aid in weight loss, providing additional benefits for people with Type 2 diabetes.
Insulin Therapy for Type 1 Diabetes and Advanced Type 2 Diabetes
Insulin Injections:
For people with Type 1 diabetes and those with advanced Type 2 diabetes whose bodies cannot produce enough insulin, synthetic insulin injections are necessary. There are different types of insulin (rapid-acting, intermediate-acting, and long-acting) that can be administered at specific times to manage blood sugar throughout the day and night. Adjustments in dosages allow for a personalized approach based on the individual’s daily activities, diet, and blood sugar levels.
Insulin Pumps:
An insulin pump is a device that delivers a continuous, adjustable dose of insulin through a small catheter placed under the skin. This device mimics the body’s natural insulin release and can provide better blood sugar control, especially for people with Type 1 diabetes or those with advanced Type 2 diabetes. Pumps allow for precise insulin delivery, making it easier to manage blood sugar fluctuations, particularly around meals and physical activities.
These treatments offer a range of options for managing diabetes effectively and are often combined with lifestyle adjustments to provide comprehensive blood sugar management. Regular monitoring and medical guidance are essential to tailor these treatments to individual needs and minimize the risk of complications.
Read More: Know What A1c Test Measures
Conclusion
The connection between insulin resistance and diabetes is crucial to understand, especially with the rising prevalence of type 2 diabetes. Insulin resistance can lead to severe health issues if not managed proactively, but lifestyle changes can often delay or prevent its progression to diabetes. By maintaining a balanced diet, exercising, and managing stress, individuals can support their insulin sensitivity and keep blood sugar levels in check.
Diabetics, depending on the type and stage of diabetes, may need different treatments to manage insulin levels effectively. For people with type 2 diabetes, early lifestyle intervention is often the key to reducing insulin resistance, while those with type 1 diabetes rely on insulin therapy to regulate blood sugar. Whether you’re at risk of developing insulin resistance or managing diabetes, understanding these connections and taking appropriate action can lead to better health outcomes.
FAQ’s(Frequently Asked Questions)
Insulin resistance occurs when the body’s cells don’t respond effectively to insulin, causing the pancreas to produce more insulin to compensate. Over time, this can lead to higher insulin and blood sugar levels, eventually progressing to Type 2 diabetes if not managed, as the body struggles to regulate glucose effectively.
Yes, insulin resistance can exist without the development of diabetes. It’s a precursor to Type 2 diabetes, but not everyone with insulin resistance will develop the condition. With lifestyle changes such as better diet and exercise, insulin resistance can be managed or even reversed before it leads to diabetes.
Yes, insulin plays a crucial role in diabetes. In Type 1 diabetes, the body doesn’t produce insulin, while in Type 2 diabetes, the body becomes resistant to insulin. Both conditions result in the body’s inability to regulate blood sugar levels properly, which leads to high blood glucose and other related health complications.
Yes, insulin resistance can lead to higher blood sugar levels. When the body’s cells don’t respond effectively to insulin, glucose remains in the bloodstream instead of being absorbed by cells for energy. This results in elevated blood sugar levels, which over time can contribute to the development of Type 2 diabetes.
Common signs of insulin resistance include increased hunger, frequent thirst, fatigue, difficulty losing weight (especially around the abdomen), and darkened skin patches (acanthosis nigricans). If you experience these symptoms, it’s important to consult a healthcare provider for testing, such as fasting insulin or glucose levels, to determine insulin resistance.
Fasting can help improve insulin sensitivity for some people by allowing the body to reset its glucose and insulin levels. Intermittent fasting, in particular, has shown promise in reducing insulin resistance and improving blood sugar control. However, it’s important to consult a healthcare provider before starting any fasting regimen, especially if you have existing health conditions.
Disclaimer
This site provides educational content; however, it is not a substitute for professional medical guidance. Readers should consult their healthcare professional for personalised guidance. We work hard to provide accurate and helpful information. Your well-being is important to us, and we value your feedback. To learn more, visit our editorial policy page for details on our content guidelines and the content creation process.

 English
English